ADA Detection: Sample Collection, Processing, and Analysis
"Anti-drug antibodies" (ADA) typically refer to antibodies produced by the immune system against certain drugs, especially biologics. When patients receive certain biological treatments (such as monoclonal antibody therapy), their immune system may produce these antibodies, which may affect the safety and effectiveness of the drugs. ADA testing is done to determine whether these anti-drug antibodies exist in the patient's body. The collection and handling of samples is very important as it can affect the accuracy of the test results.
Routine Steps for the Collection and Handling of ADA Testing Samples
1. Sample Selection
Whole blood, serum, or plasma are typically used as samples for ADA testing.
2. Sampling
Blood is collected using an appropriate blood collection tube (such as anticoagulant-free or EDTA-containing).
3. Handling
(1) If using serum: Allow blood to clot at room temperature for 20-30 minutes, then centrifuge and take the upper layer of serum.
(2) If using plasma: Centrifuge and take the upper layer of plasma.
4. Storage and Transport
Samples should be quickly frozen and stored at a low temperature (such as -20°C or -80°C). If transportation is needed, ensure that samples are transported under cold chain conditions.
5. Analysis
Once the sample arrives at the laboratory, various methods can be used for the quantitative or qualitative detection of ADA, such as enzyme-linked immunosorbent assay (ELISA).
6. Result Interpretation
Test results are interpreted based on the presence or absence of antibodies and their concentration. The presence of antibodies may be associated with a decrease in drug efficacy or an increase in adverse reactions.
In conclusion, when conducting ADA testing, the handling and analysis of samples are critical and must strictly follow standardized procedures to ensure the accuracy and consistency of the results.
MtoZ Biolabs, an integrated chromatography and mass spectrometry (MS) services provider.
Related Services
Antibody Characterization Service
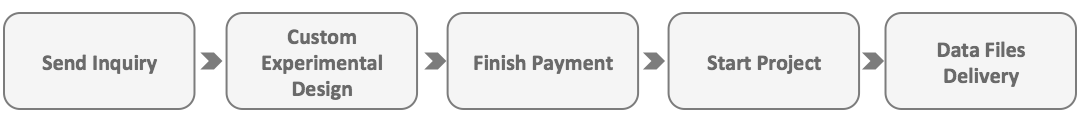
How to order?